Affiliated with Dr Samuel Duff
Before Surgery
Fasting
No food for 6 hours before surgery.
You may drink clear fluids (water, black tea/coffee without milk, clear apple juice) until 2 hours before.
Medications
Most regular medications can be taken as usual.
Patients with diabetes or on blood thinners may need changes - these will be discussed individually.
Blood thinners
Except for aspirin, all blood thinners (Warfarin, Eliquis, Xarelto, Pradaxa, Plavix) need to be stopped before surgery - usually 3–7 days depending on the drug.
Fish oil and turmeric should also be stopped.
Diabetes medicines
Do not take diabetes tablets on the day of surgery.
Some medicines (Jardiance, Forxiga, Xigduo, etc.) need to be stopped 3 days before.
No insulin on the day of surgery. If you take night insulin (like Lantus), take half your usual dose the night before.
Pre-operative consultation
You may be contacted by the pre-op nursing team or a peri-operative physician.
I may also contact you before surgery to discuss your plan and answer questions.
-
If you are taking Ozempic, Wegovy, Mounjaro, Trulicity or similar medications before surgery, you will need to follow special fasting rules.
- 24–6 hours before surgery: clear fluids only.
- 6–2 hours before: water only (max 200 ml per hr).
- 2 hours before: nothing by mouth.
Clear fluids include water, black tea/coffee (no milk), clear apple juice, electrolyte drinks, or clear broth. Avoid milk, smoothies, protein shakes, creamy soups, or juices with pulp.
If you did not follow these instructions, please tell me - your surgery may be delayed or modified.
Some conditions (e.g. gastroparesis, Parkinson’s, bowel problems) may also slow stomach emptying, even with correct fasting. Please let your me know.
Anaesthetic Plan
Your anaesthetic will usually be a combination of a general anaesthetic and local anaesthetic to provide both safety and comfort.
This often includes:
1. Spinal injection - a single injection in the lower back to numb your legs.
2. General anaesthetic (or deep sedation) - you’ll be fully asleep or very deeply sedated during surgery.
3. Local anaesthetic catheter - a soft plastic tube placed under ultrasound guidance, delivering numbing medicine continuously into your leg via a small portable pump.
This approach ensures effective pain relief after surgery, supported by pain tablets as needed.
After Surgery
You will usually receive a continuous infusion of numbing medicine into your leg, combined with pain relief tablets.
Your comfort will be reviewed daily by the Acute Pain Service team, who can adjust your medications if needed.
Common medications may include:
Paracetamol (regular simple pain relief)
Celecoxib (Celebrex) for inflammation (as tolerated, up to 6 weeks)
Tapentadol (Palexia) SR regularly, plus Tapentadol IR as needed for “top-ups”
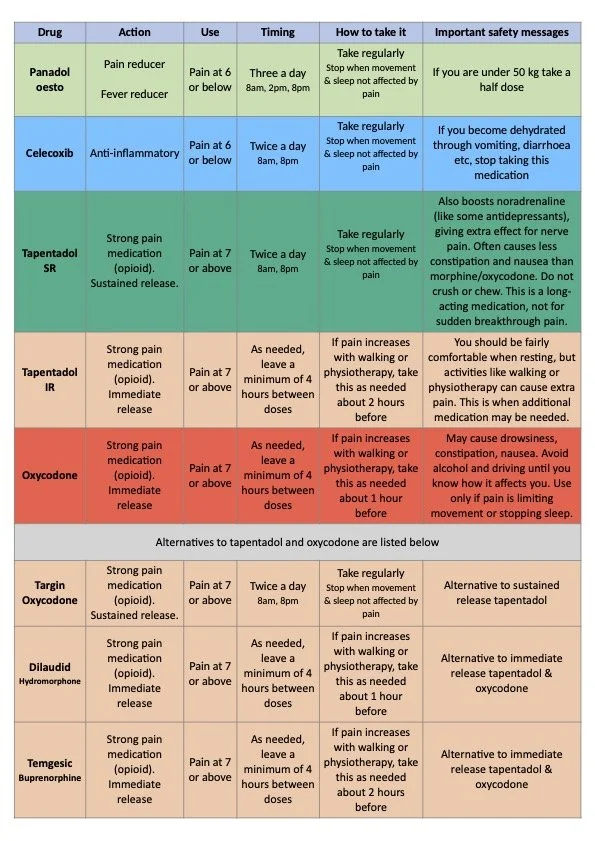
Pain Medications
You will usually go home with:
Paracetamol (about 100 tablets)
Celecoxib (about 42 tablets)
Tapentadol SR (about 56 tablets)
Tapentadol IR (about 40 tablets for breakthrough pain)
It is recommend you book in with your GP at about 4 weeks after discharge so that you can receive further scripts as required. Ideally you should not require any SR (sustained/slow release) pain killers after 6 weeks and almost certainly beyond 3 months.
Most people find their knee is comfortable at rest, but pain is more noticeable with movement, especially bending and during exercises with the physiotherapist. The goal of your pain management is to keep you mobile, so that you can walk reasonable distances and carry out your normal daily activities. It is common to have some pain at night and disrupted sleep for several months after surgery, though this does gradually improve. Below is a typical pain plan, with a detailed version available as a PDF via the button at each stage.
Week 1–2 - Early stages of recovery
Regular Paracetamol and Celecoxib.
Tapentadol SR twice daily.
Tapentadol IR as needed for extra pain, especially after physiotherapy.
Most patients find that pain is strongest during walking and exercises. In the first couple of weeks after surgery, opioid medications can be particularly helpful to support movement and make early rehabilitation easier.
Week 3–4
Gradual reduction in Tapentadol SR.
Continue Paracetamol and Celecoxib.
Use Tapentadol immediate release (IR) only if required.
Pain will steadily improve as you recover, and everyday activities will start to feel easier. If something causes too much pain, it’s better to ease back or modify the activity rather than relying on higher doses of pain medication.
Week 5–6
Aim to reduce Tapentadol SR to night-time only, then stop.
Use Tapentadol IR occasionally if needed.
Goal is to stop all strong opioid pain medicines by week 6.
If pain is ongoing, consult your GP or surgeon.
Week 7 and beyond
Opioids should be stopped as soon as your pain allows, ideally within 6 weeks and always by 3 months, to avoid long-term problems such as dependence or chronic pain.
By around seven weeks after surgery, most tissue healing has occurred and inflammation has settled, so ongoing pain should be mild and manageable without regular opioid use. Continuing opioids at this stage can slow recovery because they interfere with the body’s natural pain control, reduce alertness and energy, and make it harder to stay active. Long-term use also increases the risk of dependence, tolerance, constipation, low mood, and poor sleep. Using immediate-release opioids only occasionally for short episodes of pain helps maintain comfort while avoiding these problems.
Pain Medication Timeline
Celecoxib After Joint replacement
Using celecoxib (Celebrex) for a few weeks after your hip or knee replacement is a common part of pain management. In appropriately selected patients, it has been shown to be safe with a very low risk of serious side effects.
What the research shows
Stomach and bowel (GI) bleeding: Very uncommon - well under 1% risk.
Heart attack or stroke: Extremely rare - far less than 1% over 6 weeks in patients without existing heart disease.
Kidney problems: Uncommon - around 1% or less, usually avoidable by staying well hydrated and keeping the course short.
Wound healing and infection: Celecoxib does not appear to hinder healing or increase infection risk after surgery.
What this means for you
For most patients, a 6-week course of celecoxib:
Provides effective pain relief
Reduces the need for stronger painkillers
Carries only a very small chance of serious complications (GI, heart, kidney, or wound-related)
Waterworks
(Passing Urine)
After surgery, numbness may make it difficult to feel when your bladder is full.
This usually returns to normal within hours.
Around 10% of patients have some difficulty passing urine at first.
An ultrasound may be used to check your bladder. In some cases, a catheter may be needed temporarily.
Sleep
Sleep disturbance is common after knee replacement and may last for weeks. Adequate night‑time pain relief is important, and problems may involve difficulty falling asleep or staying asleep.
Options that may help include:
• Optimise your regular analgesia – keep taking paracetamol and any other pain killer medicines (if appropriate) so there are no gaps in pain relief overnight.
• For sleep initiation (falling asleep): – Melatonin (immediate release) 1‑3 m g taken 30‑60 minutes before bed. This aligns your body clock but has little effect on night‑time awakenings.
• For sleep maintenance (staying asleep): – Pregabalin 25‑50 m g at night. This dampens nerve‑related pain, reduces nocturnal pain flares and increases slow‑wave sleep. Use 25 m g in older adults or if there is kidney impairment. – Clonidine 25‑75 micrograms at night. This suppresses night‑time sympathetic surges and can help if you wake with a racing heart or agitation. Start with 25 micrograms and increase only with medical supervision, watching for low blood pressure.
Discuss these options with your GP if sleep remains difficult. Treatment should target the underlying causes of disturbed sleep, such as poorly controlled pain and autonomic overactivity, rather than just circadian timing.
Anaesthetic Risks
Anaesthesia is very safe, but like any medical procedure, risks can occur.
Common (5–25%)
Nausea, sore throat, dizziness, urinary difficulty, sleep disturbance.
Uncommon (<5%)
Severe pain immediately after surgery, confusion, hallucinations, dental injury, eye irritation, blood clots.
Rare (<1%)
Airway emergency, aspiration of stomach contents, severe allergic reaction, permanent nerve injury, infection or bleeding at block sites, heart attack or stroke, fat embolism.
Death directly related to anaesthesia is extremely rare (~1 in 60,000).